- Share on Facebook23
- Share on Pinterest
- Share on Twitter
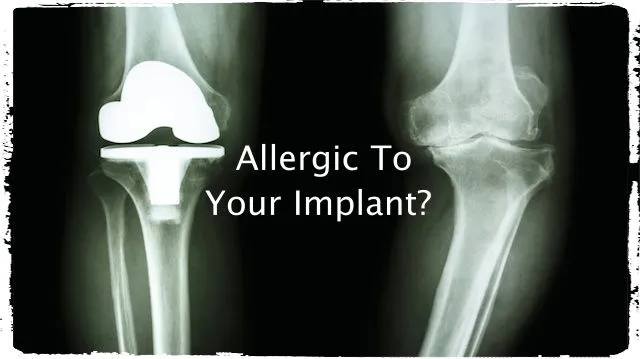
Many orthopedic surgeries commonly involve metal implants, some of which can trigger allergic reactions in sensitive people. What is even more disconcerting, the same people are subsequently at a higher risk of developing a rare, aggressive type of skin cancer.
Metal alloy implants cause allergic reactions in sensitive people
Metal alloys are used in orthopedic implants for strength and durability. Unfortunately, people who are sensitive can suffer chronic inflammation from the chromium, nickel, or cobalt often used in them. This chronic inflammation opens the door to developing skin cancer.
“Allergen-free versions of some implants are available,” said Shadmehr Demehri, dermatologist and postdoctoral fellow, and lead author of a study on the subject. “These versions may cost more or be less durable, but for some patients with sensitivity to metals, they may be the best option.”
Attention was drawn to this situation when a patient underwent implantation of a metal rod to fix an ankle fracture. Following the surgery, the patient developed a rash on the skin of her ankle in close proximity to the implant location.
The chronic inflammatory cells can lead to tumor development
The rash was a result of a nickel allergy triggered by the implant. The patient underwent another surgery to have the implant removed. However, the rash remained, and some years later a very rare type of skin cancer developed at the site of the surgery. The skin cancer, formerly called Marjolin’s ulcer ended up ulcerated and causing considerable pain before it was surgically removed.
In a study conducted by Washington University in St. Louis, it was found that continued skin contact with allergens caused chronic inflammation and promoted the development of tumors. Researchers concluded surgical patients with metal implants in close proximity to the skin should be monitored for signs of chronic inflammation. The chronic inflammation related to metal implants can contribute to joint pain, swelling, and possibly increase joint fracture.
These findings will likely lead to discussions on whether patients should be tested for sensitivities to metal prior to undergoing surgery with implants. Currently, less than five percent of implant patients experience an inflammatory rash or reaction.
Mouse models used to simulate allergic reaction to metal alloys
Scientists were very surprised by the patient’s development of Marjolin’s ulcer. This form of squamous cell cancer can potentially be deadly, and the patient didn’t fit the usual risk factors of being over 50 years old, with health issues, or a history of previous skin cancers.
The researchers used mouse models to test if contact allergies from metal implants could lead to inflammation and tumor development.
 “A contact allergy is a different kind of reaction from allergies to pollen, pet dander or food,” explained senior author Wayne M. Yokoyama, professor of medicine at the School of Medicine in Washington University, St. Louis. “A contact allergy touches the skin or is close to it. Skin rash in response to nickel and poison ivy are two common examples of contact allergies.”
“A contact allergy is a different kind of reaction from allergies to pollen, pet dander or food,” explained senior author Wayne M. Yokoyama, professor of medicine at the School of Medicine in Washington University, St. Louis. “A contact allergy touches the skin or is close to it. Skin rash in response to nickel and poison ivy are two common examples of contact allergies.”
The study found that what promoted skin tumors was the combination of contact allergy inflammatory cells along with different molecules and inflammatory cells activated from the long-term reaction.
Mouse model reproduced very similar results
“This model supported cancer development so strongly that some mice developed invasive squamous cell skin cancers similar to the patient’s tumor,” said Demehri.
“If you’re allergic to something, the first thing to do is to avoid it, but the patient couldn’t,” Yokoyama said. “Some nickel had likely seeped from the implant into her tissue and was still present in her skin even after the implant was removed. It’s as if a patient allergic to poison ivy kept putting poison ivy on the skin.”
Researchers are now trying to identify the molecules and cells responsible for promoting the cancer tumor development.
—The Alternative Daily
Sources:
http://www.futurity.org/allergy-metal-implants-skin-cancer-782042
http://www.jci.org/articles/view/77843
http://www.medscape.com/viewarticle/742801_4
- Share on Facebook23
- Share on Pinterest
- Share on Twitter

